The HESI Abdominal Assessment Case Study presents a systematic approach to abdominal assessment, providing healthcare professionals with essential knowledge and skills for accurate patient evaluation. This comprehensive guide explores the rationale, procedures, findings, and documentation of the HESI abdominal assessment, empowering practitioners to make informed decisions and optimize patient outcomes.
Through a step-by-step approach, this case study elucidates the significance of each step in the assessment process, highlighting the identification of normal and abnormal findings. It emphasizes the importance of thorough documentation, outlining key components and providing a sample template for effective communication of assessment results.
Introduction
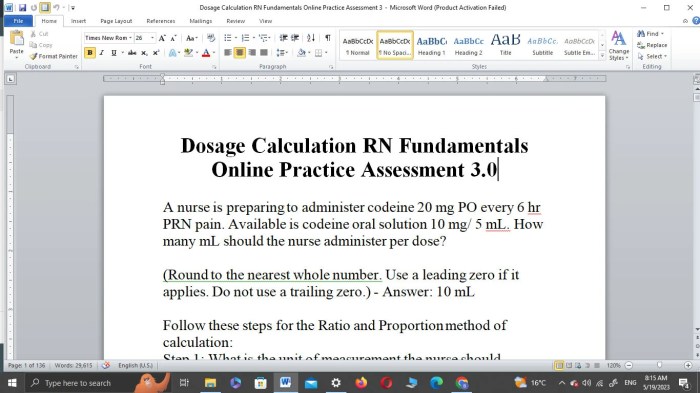
The HESI Abdominal Assessment Case Study is a standardized assessment designed to evaluate a student’s knowledge and skills in performing a comprehensive abdominal assessment.
The purpose of the assessment is to provide students with an opportunity to demonstrate their ability to:
- Gather and interpret patient history and physical examination findings.
- Formulate a differential diagnosis.
- Develop a plan for further evaluation and management.
Assessment Procedures
The HESI abdominal assessment is a comprehensive examination of the abdomen to evaluate its structure, function, and any abnormalities. This assessment is essential for diagnosing and monitoring various abdominal conditions, such as pain, inflammation, or masses.
The HESI abdominal assessment involves several key steps, each of which plays a crucial role in providing a thorough evaluation. These steps include:
Inspection
- Observing the abdomen for any visible abnormalities, such as asymmetry, bulges, or scars.
- Assessing the skinfor color, texture, and any lesions or rashes.
- Noting the presence of any pulsations, hernias, or distension.
Auscultation
- Listening to the abdomen with a stethoscopeto evaluate bowel sounds, vascular sounds, and any bruits or murmurs.
- Bowel sounds should be regular and occur approximately 5-10 times per minute.
- Vascular sounds may indicate the presence of an abdominal aortic aneurysm.
Percussion
- Tapping the abdomen with the fingersto assess the underlying structures and identify any areas of tenderness or dullness.
- Percussion over the liver should produce a resonant sound.
- Percussion over the spleen should produce a dull sound.
Palpation
- Gently feeling the abdomen with the handsto assess the size, shape, and consistency of the organs.
- Palpation can help identify any masses, tenderness, or areas of rigidity.
- It is important to palpate the abdomen in all four quadrants.
Assessment of Liver and Spleen
- Percussion and palpation can be used to assess the liver and spleen.
- Percussion over the liver should produce a resonant sound, while percussion over the spleen should produce a dull sound.
- Palpation of the liver should reveal a smooth, firm edge, while palpation of the spleen should reveal a soft, rounded edge.
Assessment Findings
When performing a HESI abdominal assessment, it is important to observe the abdomen for any abnormalities in size, shape, or contour. The abdomen should be symmetrical and have a smooth, rounded appearance. Any deviations from this normal appearance may indicate an underlying medical condition.
Normal abdominal findings include:
- Symmetrical abdomen
- Smooth, rounded contour
- No visible masses or hernias
- Normal bowel sounds
li>No tenderness or pain on palpation
Abnormal abdominal findings may include:
- Asymmetrical abdomen
- Bulges or protrusions
- Visible masses or hernias
- Tenderness or pain on palpation
- Abnormal bowel sounds
Asymmetrical Abdomen
An asymmetrical abdomen may be caused by a variety of conditions, including:
- Ascites
- Abdominal tumors
- Organomegaly
- Bowel obstruction
Bulges or Protrusions
Bulges or protrusions may be caused by a variety of conditions, including:
- Hernias
- Abdominal tumors
- Ascites
- Organomegaly
Visible Masses or Hernias
Visible masses or hernias may be caused by a variety of conditions, including:
- Abdominal tumors
- Hernias
- Organomegaly
Tenderness or Pain on Palpation
Tenderness or pain on palpation may be caused by a variety of conditions, including:
- Peritonitis
- Appendicitis
- Cholecystitis
- Pancreatitis
Abnormal Bowel Sounds
Abnormal bowel sounds may be caused by a variety of conditions, including:
- Bowel obstruction
- Ileus
- Peritonitis
Documentation: Hesi Abdominal Assessment Case Study

Thorough and accurate documentation is paramount in healthcare, serving as a vital means of communication, ensuring continuity of care, and safeguarding patient safety. In the context of abdominal assessment, proper documentation provides a comprehensive record of the patient’s condition, the findings of the assessment, and any interventions or recommendations made.
The key components of abdominal assessment documentation include:
- Patient’s personal and demographic information (name, age, medical record number)
- Date and time of the assessment
- Reason for the assessment (e.g., abdominal pain, distension, trauma)
- Detailed description of the assessment findings, including:
- Inspection: contour, symmetry, scars, distension, hernias, visible pulsations, visible peristalsis
- Auscultation: bowel sounds, bruits, vascular sounds
- Palpation: masses, tenderness, rigidity, hepatomegaly, splenomegaly
- Percussion: tympany, dullness
- Assessment of the patient’s overall comfort and pain level
- Recommendations for further diagnostic tests or interventions (if necessary)
- Signature and credentials of the healthcare professional performing the assessment
Case Study Application
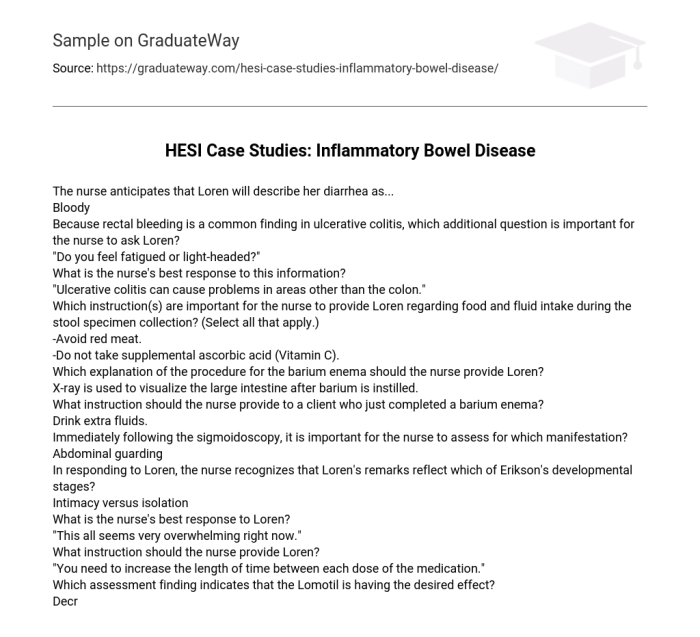
The HESI abdominal assessment is a comprehensive tool that can be used to evaluate a patient’s abdominal health. It can be used to identify potential problems, such as pain, tenderness, masses, or hernias. The assessment can also be used to monitor the progression of a patient’s condition over time.
To apply the HESI abdominal assessment to a case study, the nurse should first gather information about the patient’s history and symptoms. This information can be obtained through a patient interview and a physical examination. The nurse should then use the HESI abdominal assessment form to guide the physical examination.
The HESI abdominal assessment form includes a series of questions about the patient’s abdomen. The nurse should ask the patient these questions and record the patient’s answers on the form. The nurse should also palpate the patient’s abdomen to assess for any pain, tenderness, masses, or hernias.
Assessment Findings
The assessment findings should be documented on the HESI abdominal assessment form. The nurse should also note any other relevant information, such as the patient’s vital signs or any medications the patient is taking.
Implications of Assessment Findings, Hesi abdominal assessment case study
The assessment findings can have implications for the patient’s care. For example, if the nurse finds that the patient has pain in the right lower quadrant of the abdomen, this could be a sign of appendicitis. The nurse would need to notify the doctor and arrange for the patient to have further evaluation.
The HESI abdominal assessment is a valuable tool that can be used to assess a patient’s abdominal health. It can be used to identify potential problems, such as pain, tenderness, masses, or hernias. The assessment can also be used to monitor the progression of a patient’s condition over time.
FAQ Compilation
What is the purpose of the HESI abdominal assessment?
The HESI abdominal assessment is a systematic approach to evaluate the abdomen for abnormalities, identify underlying conditions, and monitor patient health status.
What are the key steps involved in performing a HESI abdominal assessment?
The key steps include inspection, auscultation, percussion, and palpation, each providing valuable information about the abdominal organs and structures.
Why is documentation of the assessment findings crucial?
Documentation ensures accurate communication of the assessment results, facilitates patient monitoring, and provides a legal record of the patient’s condition.